Depressed Mood
Sad, down, tired, unmotivated, tearful, low self-esteem; thoughts that turn to guilt or pessimism. It can feel like there’s no reason to live. Patterns of sleeping and eating may change and physical pain may worsen.
Most people with depression have experienced other shades to their mood that are important to identify; such as:
Anxious Mood
Worried, nervous, tense, overwhelmed, stressed, fearful.
Irritable Mood
Easily annoyed, angry, argumentative or aggressive.
Empty Mood
Unable to find pleasure in anything, not interested in people or activities (the medical term for this is anhedonic, which means “lack of pleasure”).
Brightly Elevated Mood (or Sunny Hypomania)
Self-confident, happy, out-going, active, running on high energy and little sleep, spontaneous or impulsive, thinking quickly, creative, making lots of plans.
Darkly Elevated Mood (or Dark Hypomania)
Edgy, agitated, impulsive, impatient, irritable, distracted and unfocused, not sleeping much, anxious. making unwise choices, feeling distrustful or paranoid. Often this mood makes people want to self-medicate with alcohol, caffeine or other drugs.
Mixed State
This happens when depression overlaps with a dark mania. You may feel “tired and wired”, restlessly driven but not knowing what to do. Anxiety and irritability tend to be very high and sleep very irregular. It is very hard to concentrate.
Mood and Emotion
Moods involve more than emotions. Moods bring about changes in thought, judgment, action and the basic functions of the body. In fact, mood disorders really aren’t emotional disorders. Emotions are adaptive responses to life; all emotions are normal in themselves. In a mood disorder, people lose the ability to see their emotions in perspective and to act wisely in the face of them.
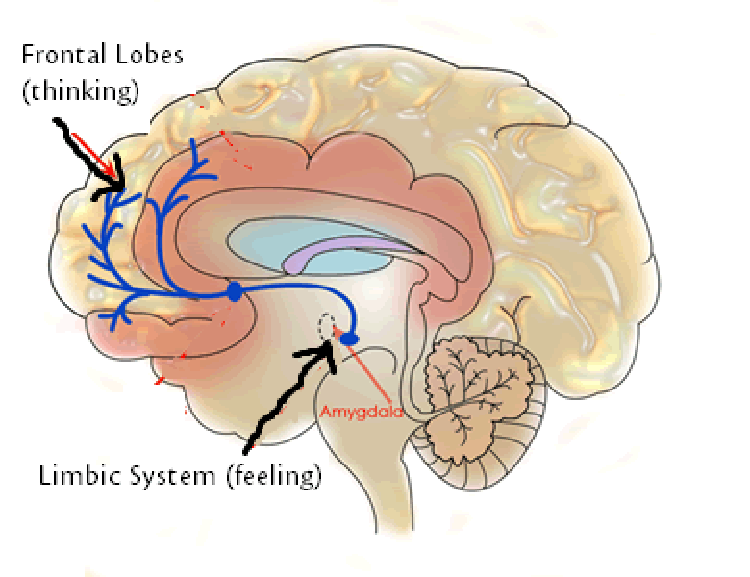
Mood disorders actually disrupt the connection between the brain’s emotional center and action center. These two parts of the brain are tightly connected, so that our actions and judgments are always influenced by our emotions (this is why we’re not like computers!). When the connection is disrupted by a mood disorder, people may act too quickly (as in mania) or not act at all (as in depression). This connection is illustrated by the blue line in the picture below:
The blue lines connect the limbic/amygdala system – which is the emotional center – to the frontal/cortical system – which is the center for action, planning, judgment.
Mood and Awareness
Your brain also has a part which makes you aware of yourself (it’s near the forehead). Some moods can make us painfully self-aware, such as the self-consciousness or anxiety or the self-critical guilt of depression. Other moods actually decrease our self awareness, much like alcohol can. These are called elevated moods and include mania, hypomania and mixed states.
Because they cloud our self-awareness, it’s rare for doctors to hear about elevated moods. Yet, research has found that identifying them is critical to recovering from depression, even if they happened long ago.
To better identify elevated moods, we’ve developed two rating scales which allow your friends or relatives to share what they’ve seen in your moods. You can also read more about elevated states here.
Mood Disorders
Mood disorders go by different names, depending on which moods occur, how severe they get, and how they change over time. Getting the right diagnosis is a critical step in finding the right treatment.
Examples of mood disorders (click title to learn more):
A depressed or empty mood that lasts at least 2 weeks. It may occur only once or keep recurring throughout life. It may go away entirely or continue at a low-grade level.
A low-grade depressed or empty mood that persists for at least two years. This occurs on a spectrum from a temperamentto a disorder.
Moods that fluctuate frequently, usually for brief periods. Any of the above moods may occur, but typically it is a depressed or empty mood alternating with an elevated or irritable one. Like dysthymia, this can be a temperament or, if it causes enough problems, a disorder.
Depressed or empty moods predominate in this condition, but there are also periods of mildly elevated mood as well (called hypomania). This condition is very common (affecting 1 in 30 people) but is often misdiagnosed as major depression.
Bipolar-I (Manic-Depression)
Depressed or empty moods alternate with extremely elevated moods (called mania).
Bipolar Spectrum
This category represents people with depression who also have other moods, but not to the extent that would qualify for bipolar-I or II. It can identify people who look like they have depression but may not respond well to antidepressants. Often people with bipolar spectrum disorder have relatives with full bipolar disorder.
Mood Changes
There are also diagnoses for how fast your mood changes: rapid cycling (at least 4 cycles per year), ultra-rapid cycling (at least 2 cycles per month) and ultradian cycling (cycling up and down within a day).
A Word of Hope
I hope you’ll remember that you are not your illness, and that even a mood disorder can be a strength. People who come out of depression often find renewed appreciation for life and more compassion for the world around them. Research has found that, despite its bleakness, depression gives people a more accurate view of reality. People with bipolar disorder tend to have greater language skills, social abilities and creativity.
Those with mood disorders are among the most creative, talented and industrious in our society. They include great leaders like Abraham Lincoln and Winston Churchill, artists and writers such as Georgia O’Kieffe, Mark Twain and Irving Berlin, and actors Robin Williams, Carrie Fisher and Ben Stiller.